Key Takeaways
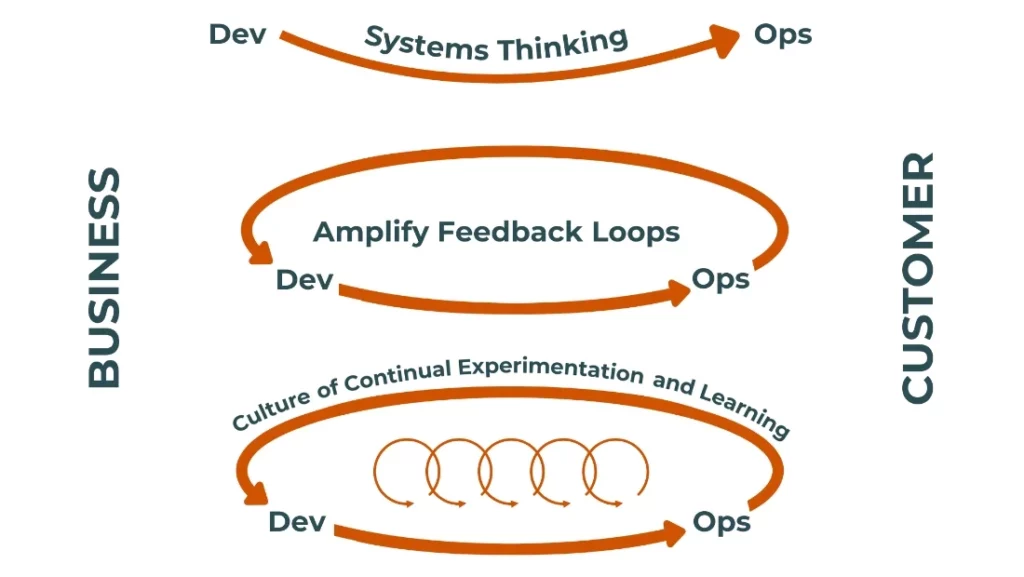
- Applying DevOps principles of flow, feedback, and continuous learning can transform medical practices into efficient, patient-centered systems.
- Automation, AI tools, and effective feedback loops streamline workflows, improve staff productivity, and enhance patient care.
- Continuous improvement through goal-setting, data-driven adjustments, and team upskilling ensures practices remain adaptable and competitive.
Running a medical practice today involves juggling countless moving parts—from managing patient flow to optimizing billing systems. It’s easy for inefficiencies to creep in, slowing down your operations and impacting patient care.
Originally designed to improve software development, these principles—flow, feedback, and continuous learning—can help you create a smoother, more efficient medical practice. They’re not just about saving time. They’re about making your practice better for patients and staff alike.
Let’s dive into how to apply the three ways of DevOps for healthcare practice management. You’ll learn how to remove constraints, establish effective feedback loops, and create a culture of constant improvement. By the end, you’ll see your practice not just as a workplace, but as a finely tuned system where every part works in harmony.
1. Establish Flow: Removing Constraints and Friction
Where Is the Bottleneck in Your Practice?
Think of your practice like a machine. Every part needs to work smoothly, or the whole system slows down. Start by mapping your workflows from end to end. This means following the patient journey from the moment they schedule an appointment to the final billing process. Break it into steps and ask yourself: where does the process stall? Are patients waiting too long for appointments? Is your staff overwhelmed with manual data entry? Identifying these bottlenecks is the first step to fixing them.
Eliminate Low-Value Tasks Through Automation
Low-value tasks are the silent productivity killers in any practice. These are repetitive jobs that don’t require human judgment, but still eat up hours of your staff’s time. Automating tasks like appointment reminders, patient check-ins, and insurance eligibility checks can free your team to focus on what they do best: patient care.
Take appointment reminders, for instance. Instead of relying on manual phone calls, use automated text or email reminders. Patients appreciate the convenience, and you’ll see fewer no-shows. Similarly, insurance eligibility checks can be streamlined with software that verifies coverage before the patient even steps into your office. It’s efficient, and it reduces billing headaches later on.
Leverage AI for Clinical Data Flow
Another example is AI-assisted translation tools. While these shouldn’t replace clinical judgment, they can help transfer documentation to other formats for use cases beyond the immediate episode of care. Implementing these tools might seem like a big step, but the payoff in time saved and accuracy gained is worth it.
How to Measure and Maintain Flow in a Medical Practice
Efficiency isn’t a one-and-done deal. Once you’ve improved your workflows, you need to track your progress. Key performance indicators (KPIs) like patient throughput, wait times, and claim rejection rates can give you a clear picture of how well your practice is running. Use data dashboards to monitor these metrics in real time.
But don’t get carried away. Over-optimization can backfire, especially in healthcare practice management. Patients are people, not numbers. Automating too much or focusing solely on speed can hurt the quality of care and patient satisfaction. Striking the right balance is essential. For example, while faster billing is great, it’s more important that bills are accurate and easy for patients to understand. Remember, the goal is to create a smoother experience for everyone, not just to move faster.
2. Establish Feedback Loops: Listening to Data and People
What Are Your Feedback Mechanisms Telling You?
The Role of Data in Feedback Loops
Data doesn’t lie. Effective ways to monitor key metrics—like average patient wait times, appointment no-show rates, and billing error rates—can give you a real-time view of how your practice is performing. For instance, if you see that wait times spike every Monday morning, you can adjust staffing levels to match demand.
Predictive analytics can take this a step further. By analyzing past data, these tools can help you anticipate patient flow and allocate resources more effectively. Imagine knowing that your patient volume will double two weeks from now. With that foresight, you can schedule additional staff or extend office hours to handle the surge seamlessly.
3. Continuously Learn and Improve: Always Striving for Better
How Can Practices Adapt and Thrive During Times of Change?
Your field is constantly evolving, and your practice needs to evolve with it. Continuous learning isn’t optional—it’s essential. Start by breaking down big goals into smaller, actionable steps. For example, if you want to reduce no-show rates by 20%, begin with simple interventions like sending automated reminders 24 hours before appointments. Track the results, then refine your approach as needed.
Looking outside of your industry can also spark fresh ideas. Activities like daily stand-up meetings, borrowed from agile project management, can streamline team communication and problem-solving. Even simple changes—like using a whiteboard to visualize daily priorities—can make a big difference.
Upskilling Teams for Long-Term Success
Your staff is your greatest asset. Investing in their growth not only improves job satisfaction but also boosts your practice’s efficiency. Offer regular training on emerging technologies, like AI-powered EHR tools or new billing software. Hands-on workshops and online courses can help your team stay ahead of the curve.
Encourage a culture of curiosity by rewarding innovative ideas. If a team member suggests a new process that improves patient check-in times, recognize their contribution. These small gestures can foster a workplace culture where everyone feels invested in continuous improvement.
A Path Forward for Your Practice
Applying DevOps principles to your medical practice can feel daunting at first, but the rewards are worth it. By focusing on flow, feedback, and learning, you’ll create a system that’s efficient, adaptable, and patient-centered. Start small, track your progress, and build on your successes. With these principles guiding your practice—paired with choosing the best partner from available physician practice management companies—you’ll be better equipped to handle challenges and seize opportunities as they come.
Explore Our Practice Management Services











